AI vs Cancer: How AI Could Redefine Breast Exams
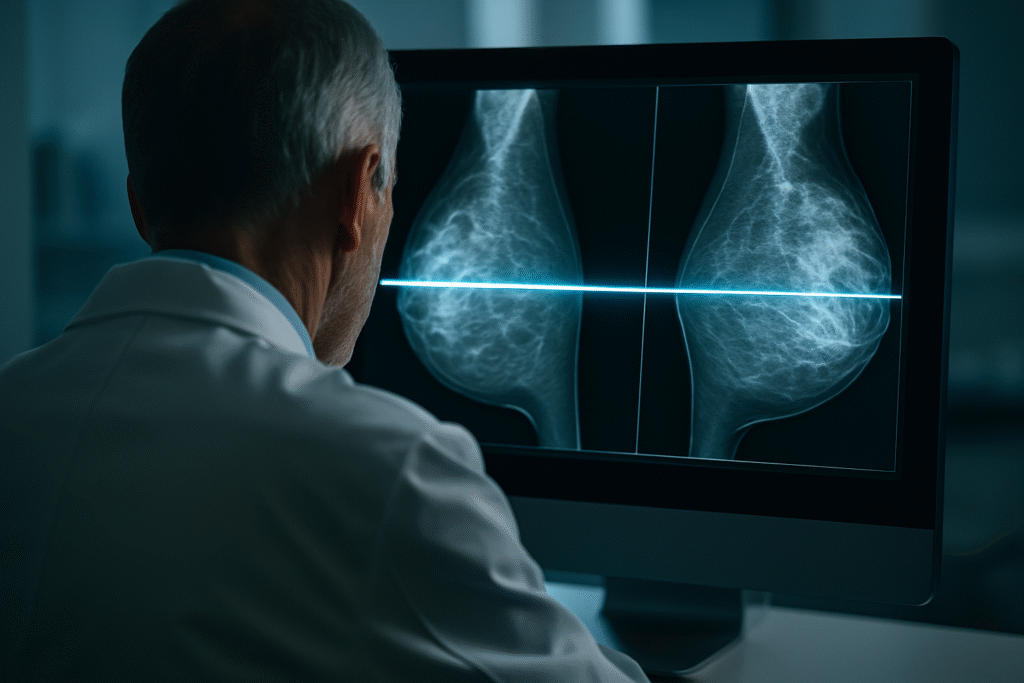
Artificial intelligence is transforming not only the tech world but also the healthcare industry. This became even clearer with a groundbreaking study published in Nature Medicine in January 2025. The use of AI in breast cancer detection via mammography is delivering faster, more accurate, and more efficient diagnoses—outperforming traditional methods.
This technology has the potential to revolutionize breast cancer screening programs globally, helping relieve overwhelmed healthcare systems and, more importantly, saving thousands of lives through early detection.
What Does the Nature Medicine Study Say?
The clinical study evaluated over 463,094 women between July 2021 and February 2023. It was conducted on a large scale, with part of the exams reviewed by AI-supported systems and the other part using traditional double-reading by radiologists.
The results are clear: the group assisted by AI achieved a breast cancer detection rate of 6.7 cases per 1,000 screenings, while the traditional group achieved 5.7 cases. This represents a 17.6% increase in detection rates, showing that AI can identify cases that could be missed by human readers.
Importantly, AI did not increase the number of false positives. The recall rate—patients called back for additional exams—was virtually identical between groups: 37.4 per 1,000 with AI versus 38.3 per 1,000 without AI.
How Does AI Improve Breast Cancer Screenings?
AI systems used in breast screenings rely on machine learning and deep neural networks. These algorithms are trained with millions of mammogram images, including both benign and malignant confirmed cases, allowing AI to detect subtle patterns and specific features related to tumors, calcifications, and other abnormalities.
Acting as a “second reader,” AI examines details like density, shape, symmetry, and texture. It highlights suspicious areas and flags patterns that might be missed by the human eye. This dramatically reduces the risk of human error caused by fatigue or oversight.
AI not only improves diagnostic accuracy but also speeds up the process. While human review may take several minutes, AI performs its analysis in seconds, freeing radiologists to focus on more complex cases.
Proven Benefits of AI in Breast Cancer Detection
- Higher detection rate: 17.6% increase in early cancer detection.
- Fewer unnecessary recalls: 2.5% reduction in the number of patients needing additional exams.
- Improved predictive accuracy (PPV): Increased from 59.2% to 64.5% with AI support.
- Reduced workload: Radiologists focus on the most critical cases.
- Standardized analysis: Reduces variability between different doctors, ensuring a consistent review process.
How Does It Compare with Other Studies?
Additional research confirms the results. AI-based algorithms are often as accurate—or even more accurate—than experienced radiologists when analyzing mammograms.
Recent studies show that multimodal models, combining 2D images, 3D scans, and digital breast tomosynthesis (DBT), achieve an AUC (Area Under Curve) of up to 0.945. This indicates extremely high accuracy, reducing false positives by up to 31.7% and saving 43.8% of healthcare professionals’ time.
In practical terms, this means thousands of hours saved in clinics and hospitals, as well as reduced stress for patients who won’t be called back for unnecessary follow-ups.
Current Challenges and Limitations
Despite the impressive results, several challenges must be addressed for widespread AI adoption in healthcare:
- Continuous medical supervision: AI is a tool, not a replacement for human judgment. Radiologists are still essential to validate results.
- Regulatory approval: Not all AI systems are certified globally. The approval process is still slow in several countries.
- Data privacy and security: Medical imaging involves highly sensitive data, requiring robust governance and security protocols.
- Infrastructure demands: Hospitals and clinics need significant investment in hardware, software, and staff training to deploy AI effectively.
Impact on Public Health and the Future of AI in Screenings
The application of AI in breast cancer detection isn’t just a technological milestone—it’s a practical solution to global public health challenges.
In countries with a shortage of medical specialists—like parts of Africa, Latin America, and Asia—AI can democratize access to accurate diagnostics. National programs like the NHS in the UK are already conducting advanced trials, showing reductions in costs, improved detection rates, and expanded capacity for public healthcare systems.
The future points to hybrid systems where humans and machines collaborate. AI handles triage, rapid analysis, and pattern recognition, while doctors focus on contextual interpretation and patient care.
Frequently Asked Questions (FAQ)
- What did the study conclude? AI increased breast cancer detection by 17.6% without raising false-positive rates.
- Will AI replace radiologists? No. AI serves as a support tool, not a replacement for medical professionals.
- Is this technology already in use? Yes. Pilot programs are running in the UK, Germany, Sweden, and even in some private clinics in Brazil.
- Is it safe to rely on AI? Yes. Studies show that AI improves diagnostic accuracy while maintaining safety, always with human oversight.
Conclusion
AI’s role in the fight against breast cancer is not just about transforming diagnostics—it’s about reshaping how we think about women’s healthcare.
The Nature Medicine study confirms that this technology is ready for large-scale deployment, offering greater safety, accuracy, and speed. However, this transformation must be implemented responsibly, with strict data protection, scientific rigor, and appropriate infrastructure.
The future of medical diagnostics has already begun—and it’s undeniably powered by artificial intelligence.